How to Read an Eob Explanation of Benefits United Healthcare
Agreement Medical Bills
Medical billing in the United states of america can seem similar an extremely convoluted process. According to a 2016 public stance survey conducted by Copatient, around 72% of American consumers are confused by their medical bills, and 94% of consumers have received medical bills they considered to be "also expensive". Fifty-fifty when covered by insurance or Medicare, you may find unexpected balances due to odd procedural codes, a slew of medical jargon, and insurance adjustments.
This guide will help you, as a patient, navigate the medical billing process from the moment you contact a healthcare provider about an appointment until afterwards you receive your bill in the mail. We discuss how healthcare providers make up one's mind costs and negotiate charges with your insurance provider. Finally, nosotros testify you how to identify and dispute erroneous charges on your bill.
What Medical Bills Really Embrace
Fees might seem capricious when you ask for price estimates from your insurer or when you lot receive a bill after your date. Withal, at that place are several elements that cistron into how hospitals, physicians' offices, and other institutions calculate the price of health services. If possible, contact your insurer to get cost estimates for multiple healthcare providers in your area. You may notice fees vary quite a bit for the same services.
In a New York Times op-ed entitled "Why Medical Bills Are a Mystery," professors Robert Kaplan and Michael Porter of Harvard Concern Schoolhouse explain that providers "assign costs to patients based on what they charge, not on the bodily costs of the resources, similar personnel and equipment used to intendance for the patient." Here are the considerations medical offices and hospitals brand every bit they negotiate with insurance companies about the costs that appear on your bill:
- Facility capacity: Hospital capacity growth is a cistron that the National Constitute for Health Care Management (NIHCM) Foundation watches closely, since the number of beds in a hospital can dramatically influence what hospitals charge nether a fee-for-service (FFS) system. Every bit hospitals add more beds, they have a greater opportunity to provide certain medical services. Equally the NIHCM notes, "Higher organization capacity tin pb to competition among suppliers and downward pressure on prices."
- Supply and demand: How readily available are the services you need? Are at that place multiple high capacity hospitals or physicians' offices in your area that can provide this service, or do you just have access to a limited number of specialists? Dr. Robert Stonebraker explains in his open source book, The Joy of Economic science, "Firms facing lilliputian or no competitive pressure are free to enhance prices well above the true cost of service. Monopoly power drives up prices in medical intendance, just every bit it would it in retailing and restaurants."
- Infirmary reputation: A hospital'southward reputation has a ripple upshot on how many patients utilise a facility, which in turn influences demand and cost. However, the Agency for Healthcare Research and Quality warns consumers that "Clinical quality scores contributed piddling to hospital selection compared with a hospital's reputation." This tin can drive business organisation and influence service costs, but yous shouldn't rely on perceived reputation as an indication of performance and quality.
- Accuse Clarification Main (CDM) lists: This resource is a master list of service costs and billing identifier codes that medical billing professionals use during the claims procedure as health offices calculate how much to bill insurance companies and patients. Each infirmary maintains its own individual chargemaster list. The American Health Information Direction Association (AHIMA) recommends that CDM prices should be maintained by chargemaster committees that oversee responsibilities like "reviewing all charge dollar amounts for appropriateness by payer."
Medical billing and coding professionals are working behind the scenes from the moment you schedule an engagement upward until y'all receive a neb. Most patients aren't familiar with the negotiations that occur between insurance companies and healthcare providers. Understanding the back and forth tin can have some of the mystery out of the insurance and billing processes.
How the Billing Bike Works
- You contact a healthcare provider. Pre-annals and provide basic information to the part, such as identification and insurance information. You schedule an appointment.
- It is of import to ask the healthcare provider about the services and supplies you'll receive. If you are not clear on upcoming charges or what insurance volition cover for the appointment, so be certain to ask for the process codes.
- Next, contact your insurance visitor to find out if these services are covered past your plan. If so, become an guess of how much the services cost with your health insurance.
- If the price is not manageable, ask your insurer if there are other healthcare providers in your area who provide the same service for less.
- The healthcare provider contacts your insurance company in order to verify:
- Preauthorization: Some insurance companies crave prior authority before they comprehend a medical service or medication. The insurance visitor collects further information regarding your engagement and medical records earlier determining whether the services and medications are covered.
- Co-Pay: The healthcare provider'south office besides determines how much the patient must pay out-of-pocket for this visit.
- On the solar day of the engagement, you consummate any boosted registration paperwork, supplying your insurance card, a valid ID, policyholder name, and your insurance group number. This registration process helps healthcare providers:
- Update your medical records electronically; pre-existing conditions can gene into coverage decisions
- Provide you with privacy policy information
- Gain your consent to perform certain procedures
- Inform you of care liability and risks
- Inform you of patient fiscal responsibilities
- Decide your advanced directive preferences, which will give healthcare providers clear instructions if you lot are unable to speak for yourself
- After services are received medical coders identify all services, prescriptions, and supplies received during your date and update your records with the respective service codes.
- The healthcare provider creates an insurance claim using these codes. They and then submit an 837 file to your insurance, the standard file format ready past the Health Insurance Portability and Accountability Act (HIPAA), allowing your healthcare provider to communicate deeply with your insurance.
- A claims processor, who works for your insurance provider, reviews the insurance merits and verifies that the treatments you've received fall under your coverage benefits. (At this point, the insurance claims processor may contact you or your healthcare provider for additional information regarding the services and/or supplies you received.) The insurance claims processor decides whether the claim is valid, and then accepts or rejects information technology.
- The insurance claims processor contacts your healthcare provider with the status decision. If the claim is valid, insurance reimburses your healthcare provider by paying for some or all of the services. If rejected, the claims processor provides the billing function with a detailed description of why the services are non covered.
- Your healthcare provider bills yous for the remaining balance.
NOTE: If y'all are 65 or older, you are entitled to federal health benefits through Medicare. This social insurance program differs significantly from individual health insurance providers when it comes to billing. Rather than negotiating prices with a healthcare provider like private health insurers, Medicare publishes set fees for services. If you are enrolled in Medicare Part B, your healthcare provider consults the Medicare Md Fee Schedule (MPFS) to determine the set price for the services you lot received.
How to Read Your Neb
One time you lot receive a medical bill from your healthcare provider, you lot volition detect that it consists of multiple components that might not be clear to you. For well-nigh patients, the codes, descriptions, and prices listed in their bills can seem disruptive.
The following example explains each element of your nib with an in-depth description. It is important not to go your medical bill confused with the Explanation of Benefits (EOB), an insurance study nosotros cover following the bill.
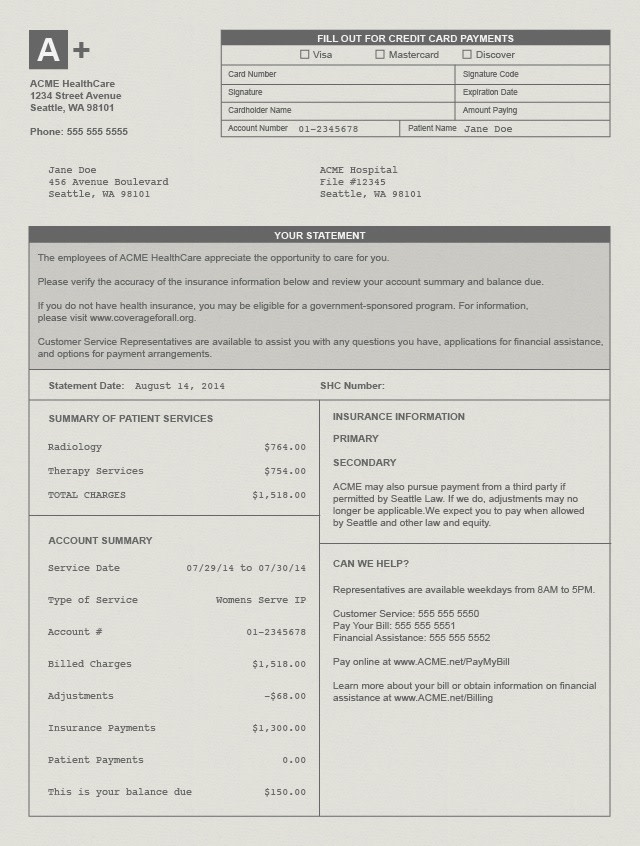
- Argument Date: The date your healthcare provider printed the bill.
- Account Number: This is your own unique account number. If you have questions regarding your bills and remainder, you demand to provide this number when contacting your healthcare provider's billing role. Account numbers are also typically used when you pay for a bill online.
- Service Appointment: Your neb includes a cavalcade listing the dates yous received each medical service.
- Clarification: This is a short phrase that explains the service or supplies you received.
- Charges: This is the full price of the services or supplies yous received earlier insurance has been factored in.
- Billed Charges: This is the full amount charged directly to either you or your insurance provider.
- Adjustment: This is the corporeality the healthcare provider has agreed not to charge.
- Insurance Payments: The corporeality your health insurance provider has already paid.
- Patient Payments: The amount you lot are responsible to pay.
- Residual/ Amount Due: The amount currently owed the healthcare provider.
- Payable to: This is the organization yous should address cheque payments to.
You lot may also come across a "service code" listed on your bill. Healthcare providers utilise a standardized Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) to identify the exact services and supplies yous received during your appointment. Annotation: Coding protocol is used internally and may not be included on your beak.
What is an Explanation of Benefits (EOB)?
An EOB is a certificate sent to insured individuals after a claim has been submitted past a healthcare provider. It explains what medical treatments and services the patient's wellness insurance company agreed to pay for and what treatments/services (if any) the patient is responsible for paying. EOB stands for explanation of benefits. It is non the same as a medical bill, although it may expect similar and show a balance due. When the EOB indicates that coin is still owed to the dr. or dentist who provided care, patients can expect a carve up bill to be sent from the dr. or dentist's role. In this instance, payment should be fabricated directly to the practitioner, not to the insurance company who sent the EOB. The purpose of EOBs is to keep consumers informed of their healthcare costs and expenditures. Information technology also offers insured customers a chance to double-check that services are billed correctly.
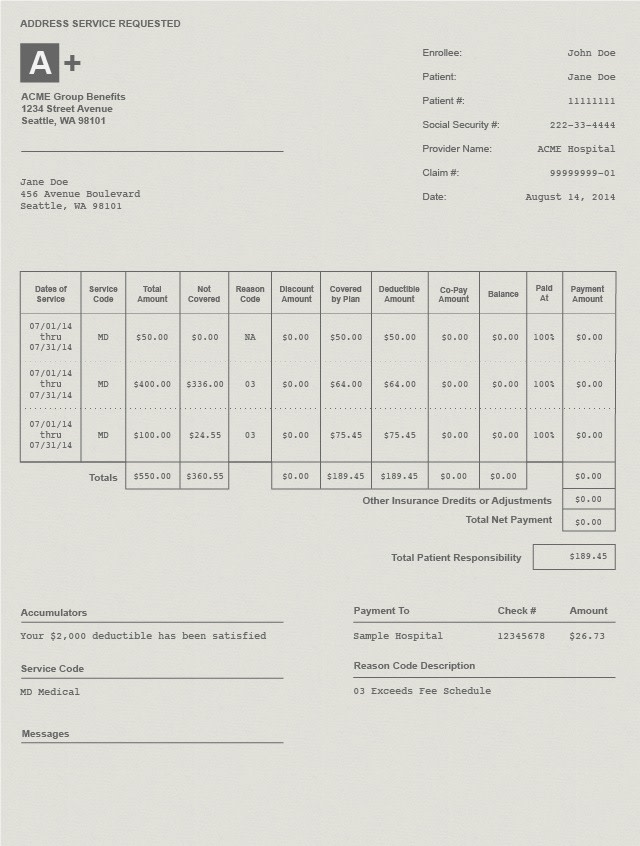
- Member Information: This shows the health insurance member's full proper name and ID number.
- Patient Account Number: This is the unique identification number used by your healthcare provider to track your account.
- Provider Name: The name of the hospital, physicians' office, or healthcare professional person you visited during your appointment.
- Merits Number: This unique identification number is used past your insurance provider to runway your business relationship.
- Appointment of service: The date yous received the medical services, procedures, or supplies.
- Service Code: This identifies the specific services, procedures, or supplies you received from a healthcare provider.
- Total Corporeality: This dollar amount shows the full cost of the procedures, services, or supplies.
- Non Covered: This is the corporeality your wellness insurance does not embrace. You are responsible for this amount.
- Reason Code Description: This lawmaking provides the reason(s) why your insurer did non cover a charge.
- Covered by Plan: This is the total amount your wellness insurance provider has saved yous.
- Deductibles and Copayments: Adjustments added based on the deductible and copay features of your insurance program.
- Total Net Payment: This includes the full dollar amount your insurance company has paid to your healthcare provider.
- Total Patient Responsibility: This is the total amount you owe your healthcare provider.
- Checks Issued: This section gives you lot a detailed record of the payment transactions from your insurer to your healthcare provider. These lists generally contain the payee's name, bank check number, and check amount.
Dealing With Billing Errors
Since medical billing processes involve several parties – y'all, your insurer, and your healthcare provider – mistakes tin and do happen. A medical coder might have inaccurately described your care history with an inaccurate code, a medical biller might have mistyped a value, or a claims adjuster might accept practical the wrong plan data to your claim. Regardless of the reason behind this error, information technology is important for you as a patient to monitor your bills and EOB forms. If you notice charges that look out of identify, do not hesitate to contact your insurers and/or healthcare providers to dispute the error.
Identifying Errors
- Compare estimates to your final bill: Earlier your engagement, contact the healthcare provider and enquire to be given the billing code and cost. Adjacent, contact your health insurance provider to make sure the process is covered past your plan and obtain an estimate of how much you lot will need to pay for the procedure. If your estimated total is very different from your balance due afterwards the appointment, at that place may be a billing error.
- Create a list of charges: Create a tape of all the medical services and supplies y'all received, forth with their corresponding charges. This tin help you identify an incorrect accuse in the future.
- Duplicate charges: If you observe the same charge listed twice, it is likely that an error occurred during data entry.
- Beware of upcoding: Upcoding is the criminal act of fraudulently reporting an incorrect diagnosis in society to profit. A disreputable healthcare provider might utilize upcoding so it receives a large payment from you or your insurance company. If a procedure description or code seems to include services you did not hold to, it could exist a form of upcoding.
- Check identifying information: Make sure your name and identification numbers are correct. Mistakes in identification could lead to insurance coverage discrepancies.
Disputing Charges
- Contact your healthcare provider's billing role: Speak to your healthcare provider nigh pecker inaccuracies. If they made an mistake during the claims procedure, they should exist able to right it. Take note of the billing representative, the date, and time of your phone call.
- Call your insurer: If you are unable to resolve the error with your healthcare provider, contact your insurer virtually the disputed charge. They can piece of work with you to file a formal appeal to dispute a accuse. They can also examine your nib for red flags that could indicate fraudulent activity committed past the healthcare provider.
- Contact a credit-reporting bureau: Make sure your disputed bills do not bear on your credit score. Every bit yous dispute a charge, your healthcare provider might mark the neb as overdue, which can impact your credit score. Your credit agency should be able to address credit score problems if you are still disputing a charge.
- Credit reporting agencies:
- Experian
- TransUnion
- Equifax
- Credit reporting agencies:
- Submitting credit complaints: Federal Trade Commission Complaint Assistant
Above all, think to non be afraid to enquire questions when at the hospital or physician'southward role; information technology is important to properly grasp what is covered by your insurance. Maintain a record of your medical bills and keep an eye out for errors and discrepancies.
mcneilhartatied1956.blogspot.com
Source: https://www.medicalbillingandcoding.org/health-insurance-guide/understanding-medical-bills/
0 Response to "How to Read an Eob Explanation of Benefits United Healthcare"
Post a Comment